Breastfeeding Information
Please note: This page has been created by Debbie Tetlow RN IBCLC, for Helensville Birthing Centre. While every effort has been made to provide evidence based and up-to-date information, it is provided for general informational purposes, does not necessarily imply endorsement by HBC, and is not meant to substitue individual professional medical advice.
Before baby arrives
Why is breastfeeding important?
Breastfeeding benefits for you
Breastfeeding:
- helps you relax and encourages a close bond between you and your baby
- helps your uterus (womb) contract after birth, so there’s less blood loss
- usually delays periods for a while. This may help prevent you from becoming pregnant again. Check out the Lactation Amenorrhoea Method
- reduces the risk of postnatal depression (also known as perinatal distress)
- reduces the risk of cervical, ovarian and breast cancer
- reduces the risk of high blood pressure and heart disease
- reduces the risk of brittle bones later in life
Breastfeeding benefits for your baby
Breastfeeding:
- is the best food (super kai!) for a baby for the first six months
- is always ready and at the right temperature
- means you can hold baby close. They love this!
- results in less tummy bugs, chest infections, ear infections, urinary tract infections and less likelihood of sepsis and meningitis
- reduces the risk of SUDI (sudden unexpected death in infancy)
- reduces the risk of allergies, eczema, asthma, and reflux
- reduces the risk of some childhood cancers, coeliac disease, and Crohn’s Disease
- reduces the risk of heart disease, obesity and diabetes in later life
- helps your baby’s brain develop
- helps with development of the jaw, teeth and speech
Breastfeeding benefits for your whānau
Breastfeeding:
- saves time – no transport, shopping, prep or cleaning up required
- saves money – you don’t need to buy formula, bottles, teats and sterilising equipment
- means you can go anywhere and feed anytime without equipment
- results in no waste – good for the environment and your budget
Covid-19 and breastfeeding – a short World Health Organisation video
The benefits of breastfeeding– a WHO graphic
Benefits of Breastfeeding – NZBA
How can I prepare for breastfeeding?
Breastfeeding is instinctive for babies, but a learnt skill for mothers. Here are some of the things you can do to prepare for breastfeeding.
- Do all you can to learn about breastfeeding before your baby arrives.
- Ask the women in your family/whānau about breastfeeding – they often have a wealth of experience and knowledge.
- Attend the Milk Cafe at our Drop in Clinic. Watching other women breastfeed their babies is a very natural way to learn and helps create supportive connections for later.
- You can learn a lot about breastfeeding by attending The Helensville Birthing Centre pregnancy and parenting classes.
Talk to your midwife during your antenatal visits and discuss what will happen in the early days after the birth. If you have any worries (like inverted nipples), make sure your midwife knows and you get the chance to talk about it. You can also watch a selection of videos from Best Beginnings “From Bump to Breastfeeding”
- Wearing maternity bras during your pregnancy will help get your bras softened and comfortable for the early days of breastfeeding when nipples can be tender. Your milk-making breast tissue grows during pregnancy. If your breasts increase by around one bra cup size, this tells you that you have a normal amount of milk-making tissue. It also tells you that you can make a normal amount of milk. Your breasts will get bigger too, after your baby is born. Tight bras are not comfortable so make sure yours have enough room.
- You don’t have to toughen up your nipples for breastfeeding.
You can massage your breasts and express a small amount of colostrum (the first milk your baby gets) in the last weeks of pregnancy. This first milk (also known as liquid gold because it can be yellow) is thick and protects your pēpi from infections. Massaging your breasts gets you used to handling your breasts and nipples and encourages colostrum production. See also: How do I hand express my breastmilk and antenatal hand expression.
- Encouraging your colostrum production will make life easier for both of you in the first days.
- You can also collect and freeze colostrum for when your baby comes. Storing Breastmilk. You can discuss this with your midwife.
- Talk to your partner and family about your breastfeeding goals. Partner support is the most significant factor for breastfeeding success.
- Plan your maternity leave (as needed).
See a lactation consultant if you have any concerns.
Useful sources of breastfeeding information
Check out these local and international websites for more useful information about breastfeeding.
- BreastFedNZ (free app)
- KellyMom
- La Leche League NZ
- La Leche League international
- NZ Breastfeeding Association
- NZ HealthEd
- UNICEF Baby Friendly
Some useful sites for dads
Do labour medications, or the type of birth, affect breastfeeding?
Many medications used in hospitals, and a difficult birth, can make it difficult for a baby to feed well in the first few days. The milk may also be late coming in.
A drug-free vaginal birth, is the best start to breastfeeding. During your pregnancy you can discuss with your LMC how to plan for a vaginal birth and drug-free ways to cope during labour.
Sometimes birth interventions are beyond our control. If this happens, lots of skin to skin in the early days and hand expressing of colostrum to feed your baby is the best way to help.
Breastfeeding challenges in the early days
Several factors can create breastfeeding challenges – many are outside your control. They include:
- no breast changes during pregnancy
- inverted nipples
- hormonal or metabolic conditions. For example, PCOS (polycystic ovary syndrome) and insulin dependent diabetes.
- being overweight or a high BMI (body mass index)
- the use of recreational drugs (including cigarettes and alcohol) or the abuse of prescription drugs
- previous breast surgery
- being an older first-time mum, for example 35 years +
- IVF (In Vitro Fertilisation)
- birth interventions including the use of medications during inductions, managed labours and births, for example prostaglandins, Syntocinon, and Syntometrine. Also intravenous fluids, pethidine, an epidural, or forceps, ventouse or a caesarean birth.
- a difficult birth, separation of a mum and baby, an unwell mum or baby, a baby smaller than 2,500 grams, or born before 38 weeks, or a tongue-tied baby can all lead to breastfeeding challenges.
Don’t worry – there’s good news. Every breastfeeding pair is unique and not everyone is affected by the same issues in the same way.
If you and your baby have experienced some of the risk factors listed above, you can take several simple steps to help.
Before baby is born
- Massage your breasts and hand express colostrum in the weeks before your baby is born.
- Collect and safely store colostrum for use during the first few days.
- If your nipples are flat or inverted, talk to your midwife and/or lactation consultant for advice.
- Plan for a vaginal, drug-free birth, if possible.
After the birth
- Enjoy lots of skin to skin with your baby. You could use a wrap for continuous skin-to skin kangaroo care style. Watch this video on how to do this safely.
- Encourage your baby’s instincts and reflexes to feed using the biological position.
- Breastfeed early and often while using breast compressions.
- Hand express colostrum after feeds or feed attempts.
- Use a breast pump for extra stimulation after feeds or feed attempts.
- Give your baby your breastmilk only, unless on medical advice.
- Ask for help from your midwife and/or a lactation consultant.
Even if the start of your breastfeeding journey is challenging, with time and support most people find breastfeeding becomes easier and more enjoyable.
This short video from the Unicef UK Baby Friendly Initiative talks about the best ways to support new mothers with feeding.
Infant formula
According to the World Health Organization (WHO) globally: “If every child was breastfed within an hour of birth, given only breast milk for their first six months of life, and continued breastfeeding up to the age of two years, about 800,000 child lives would be saved every year.”
When breastfeeding, it’s not recommended to give your baby extra fluid (either formula or water) as this can affect your milk production, expose your baby to a foreign protein (and increase the chances of developing an allergy), and may make your baby less willing to feed from the breast.
For certain medical reasons, you may need to give your baby a supplementary feed. The WHO recommends breastmilk from another healthy woman is preferable to infant formula. What you feed your baby is always your choice.
The following information can help you make an informed choice about using breastmilk from another mother:
Sharing Breastmilk- Waitemata District Health
Human milk for human babies
Human milk for human babies – Facebook NZ
The following information can help you make an informed choice about using infant formula:
14 Risks of Formula Feeding
21 Dangers of Infant Formula
The Risks of Not Breastfeeding for Mothers and Infants
Feeding your baby infant formula
Infant formula and responsive bottle feeding
Should I give my baby Follow On Formula
Your lead maternity carer (LMC) and Helensville Birthing Centre staff will support your choice of feeding and help you with what you need to know.
Dummies and teats
Babies use different muscles when sucking on bottle teats because they are very different to breasts. This means that they develop a different technique and sometimes over strengthen certain muscles. This can result in sore nipples and cause your baby to get frustrated when back at your breast.
It’s best to avoid teats and dummies for at least the first four to six weeks. If you really need to use them, choose those that are big or long so your baby has a big mouthful, and isn’t practising a really shallow latch. Avoid those that look like a badly misshapen nipple (the so-called orthodontic teats) unless you want your baby to expect and practise that!
Bottles, dummies and teats can also be a common source of thrush infections.
Breastfeeding diet and nutrition
Are there foods I should avoid?
No. Your baby will have enjoyed all sorts of flavours during your pregnancy, as the fluid around your baby picked up the flavours of the food you ate. Your breastmilk will be the same. This is good for your baby’s development.
Everything in moderation is a good approach.
Very small amounts of caffeine pass through to your breastmilk. Some babies are sensitive to this, and it may keep them awake. See: caffeine and energy drinks
Are there foods I should eat?
No special foods are required. Your breasts will always make good milk, just like your body always makes good blood. Eating nutritious food makes good sense for your own health and energy.
Making breastmilk consumes around 500 calories and 25gms of protein; and tiny amounts of trace elements per day.
For practical suggestions go to Eating for Healthy Breastfeeding Women.
If you are vegan you will need to take care to get enough vitamin B12, calcium and zinc. A lack of Vit B12 can be very serious for a baby.
For practical suggestions on what to eat go to Eating for Healthy Vegetarians and the Vegan Society
The first few days
Why’s skin to skin so important?
Skin to skin helps steady your baby’s breathing, heart rate and temperature. It helps with bonding, breastfeeding and protecting your baby from infections. Your baby will be calmer and less likely to cry.
It also helps your placenta come out, increase your breastfeeding hormones, and helps you feel calm.
When babies are skin to skin, they use all their five senses, especially smell and touch, to find your breast and latch on. Your baby will take short rests too. Many babies will manage this, all on their own, within the first hour after birth.
This can be a wonderful time for you and your baby to recover and get to know each other. A breastfeed during this first hour is especially good for your baby and your milk production.
Some babies can be sleepy or have difficulty feeding due to labour medications or a difficult birth. This is when it is good to express some of your milk to give to your baby (see How do I hand express my breastmilk).
Skin-to-skin is important at any time – not just straight after the birth.
Discuss skin-to-skin with your whānau and support people, so they know how important it is, and can help.
Discover more about skin-to-skin with these resources:
Keeping your baby skin to skin
Dr Nils Bergman on skin to skin
Skin to skin – for you and your baby at Helensville Birthing Centre
What to expect in the first week
A big change for baby
Your baby will want to be held a lot, and not sleep for long (if at all) in a bassinet. This is to be expected. It is not a bad habit. Skin-to-skin care, and your voice, helps reassure your baby that they are safe.
And big changes for you…
Feeding
Your baby will need to feed frequently, especially at night. Newborns feed the most between 9pm and 3am. During the second night, it may seem non-stop. Feeding at this time is important. Colostrum volumes are very small, but perfect for baby’s small tummy. Lots of this time at your breast tells your breasts to produce more colostrum.
Tiredness
You will be tired from the labour and birth and caring for your baby through the night. Visitors will need to know that it is vital for you to catch up on sleep during the day.
A big learning curve
In the first few days you are learning how to:
- position yourself and baby comfortably
- cope with the frequent feeds, tender nipples, and helping a baby get colostrum (and supporting milk production).
Your milk usually comes in on the third day, but is sometimes delayed.
Mixed emotions are normal
You may feel elated and in love with your baby. You may also feel tired, overwhelmed, sore, and anxious at times. Day three especially, is known for the baby blues.
If the blues don’t go away, you may be developing postnatal depression. You can discuss this with your midwife or read more about this here. Postnatal depression can be treated and you can get the support you need to feel well again.
How do I help my baby breastfeed?
Breastfeeding is instinctive for babies. But for mums, it’s more of a learned skill where confidence comes with practice. In a few weeks you’ll usually find it heaps easier.
Babies are born with many reflexes to help them find the breast, latch on and feed. These are:
- arm and leg circling
- head bobbing
- rooting – turning head from side to side, especially if anything touches the cheek
- gape – your baby will open their mouth and tilt their head back into the drinking position when something brushes their top lip
- extrusion – your baby will open their mouth and their tongue will come forward when something brushes their bottom lip
- suck – your baby will begin to suck when something touches the roof of their mouth.
Your baby can make the best use of these reflexes when on their tummy. Understanding and practising this with your baby can help breastfeeding get off to a great start.
Other important things to understand
- Babies find the breast by smell and feel, searching for the breast with their face. If they can’t feel with their face, they will use their hands.
- Use your hands or arms to help your baby feel stable and secure.
- A baby will often vocalise during this time. Your voice will be reassuring and encouraging to your baby.
- It’s helpful if feeds are as often and as long as your baby wants (it’s not helpful to watch the clock or set a timer).
- It’s usual for a newborn to feed between eight to 12 times a day.
- Most feeds will be at night as newborns feed the most between 9pm and 3am!
How do I latch my baby on?
Latching step by step…
- Have your baby skin to skin as much as possible and respond to early cues.
It’s best if your baby is hands-free and not wrapped in a blanket when feeding, so that they can get close and snuggly with you, tummy to tummy. - Make yourself comfy and in a supported position. An incline of around 45 degrees works well. Place a pillow behind your back, so that your back is not curled around in a C shape. This allows your baby to have contact with lots of your body and it makes your nipples point out at a helpful angle. If your nipples point down, it can be tricky for your baby to latch. A small rolled up cloth under your breasts will lift them up a bit.
- Have your baby on their tummy on top of you with arms and legs in a crawling position. This supports them to feel secure and use their inbuilt reflexes.
- You can ‘shape’ your breasts a little so that the nipple feels really obvious to your baby and so that they get a big mouthful when landing on it… as long as you don’t move your breasts from where they naturally sit. This ‘shaping’ is much the same as how we shape a burger or sandwich to get our mouth around it. Instead of putting your nipple in your baby’s mouth, help your baby take the nipple. Talk to your baby to help them stay calm. Your baby will likely latch all on their own. Babies often wriggle and shuffle to adjust their position and latch, and they like to have their feet in contact with something. Babies use their hands to help themselves too.If your baby can’t latch, give them some expressed colostrum (maybe on a spoon). Having some ready is helpful.
Sometimes after having a little colostrum a baby is ready to try again. You can try different positions such as the side-lying position.
If your breasts are very full, express a small amount of milk which may soften the breast enough to help baby latch.
If after about 15 minutes of trying, your baby isn’t successful, it’s best to hand express and give your baby what is available on a spoon. It’s not helpful if either of you get tired and stressed. There are many reasons why a baby can find feeding difficult in the first few days. It absolutely does not make them a ‘bad’ or ‘naughty’ baby, or you a ‘failure’!
If you find latching is often difficult, ask for help from your midwife or a lactation consultant.
Here’s some great further reading (or listening) around breastfeeding positions:
How to awaken your baby’s breastfeeding instincts
Laid back breastfeeding
What happens when mothers lie back
Improving latch by improving positioning
Biological Nurturing
Getting Help
Support from other mums
We encourage you to connect with other breastfeeding mums and join the wider breastfeeding community – both in Aotearoa, New Zealand and internationally.
Below are some of the ways you can find support on your breastfeeding journey:
Helensville Birthing Centre Peer Supporters
Helensville Breastfeeding Support Facebook page
La Leche League NZ Breastfeeding Support Facebook page
La Leche League NZ Online Meeting Facebook page
Breastfeeding NZ Facebook page
La Leche League email support
La Leche League text support – 020 4116 9994
Support from lactation consultants
You can access support from lactation consultants through the Helensville Birthing Centre before, during and after your stay, and at any time in your breastfeeding journey. This service is free for local women in the South Kaipara area (from Riverhead to Glorit).
- Visit Lactation Consultant Clinic for more information
- Find a Lactation Consultant outside the HBC area
- Healthpoint Breastfeeding Support Directory
Knowledge and Skills
How do I know if my baby is feeding well?
How long should I feed?
Somewhere between five and 30 minutes is normal. Babies have different size feeds, just like us. Sometimes they have a quick drink to quench their thirst or for a snack; other times they want a whole feast. “Watch your baby, not the clock” and let your baby feed until they seem done.
How often?
Babies usually need to feed at least eight times in each 24-hour period.
At the beginning, your baby will need to feed very often because their tummy is tiny – a one-day-old baby’s tummy only holds about a teaspoon, so a few drops to a teaspoon of colostrum is enough to start with.
What’s more, colostrum and breastmilk are digested quickly. Frequent feeds are also the way to stimulate your breasts to produce more milk.
What’s the break between feeds?
The gap between feeding times can vary greatly – maybe from 30 minutes to four hours. Babies also usually don’t feed at regularly spaced intervals but might go longer between feeds in the morning and less time between feeds in the evening.
Having fixed ideas about feeding or trying to force your baby to feed to a schedule can cause problems. You can read this blog from UNICEF on stretching out feed times.
How often a baby needs to feed is also related to how much milk a mum can store. This varies between women, and between breasts. (You can’t tell simply by looking at the breasts.)
For one mum, the production might slow right down (because her breasts are getting full) when there is maybe 40mls of milk stored. For another mum, the production might only slow down when there is around 80mls stored.
Both these mums can make the same amount of milk over 24 hours, but the mum with the smaller storage will need to remove milk twice as often. Her baby’s feeds will probably be quicker, and even look like snack feeds – it doesn’t matter. In fact, the mother of this baby is likely to spend less time on winding, baby’s discomfort and mopping up sicky spills, than the mother whose baby has fewer, but bigger, feeds.
Milk production slows as breasts fill – a necessary feedback loop.
How do I know if my baby is getting enough?
Your baby’s wee and poo and weight gains can give you a good idea of how much milk your baby is getting. Below is a chart of what you can expect.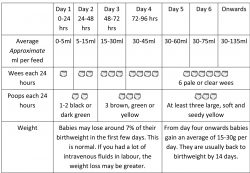
You may experience a delay with your milk coming in. This is temporary but may knock your confidence. When your milk does come in, you’ll usually notice lots of it.
You might worry that you are not producing enough milk if your baby is unsettled or feeding frequently, but this can be normal for babies.
Babies can have growth spurts or frequency days and need to feed more often to increase your milk production. This can happen every few weeks in the early stages of breastfeeding. Letting your baby feed often will soon increase your milk production.
Here’s some numbers
The un-stretched tummy of a one-month-old is about 40mls, whereas the un-stretched tummy of a six-month old is about 100mls. Their tummies can stretch to hold more, but there may be discomfort and spilling.
After the initial weeks, once breastmilk production has ‘got up to speed’ the average amount for each 24 hours is about:
- 750 ml of breastmilk (range 570-900 ml)
- 10 feeds
- 75mls per feed
- 155-240 gms weight gain each week until four months old then 95-125 gms each week until six months old.
If you think you need to give your baby additional milk it’s a good idea to talk with your health professional.
It’s best to give the smallest amount that your baby might need, while working on ways to increase your milk production.
You don’t need to give extra milk at each feed, nor does your baby need the same volume of milk each time. Be guided by your baby’s satisfaction and the plan you made with your health professional. You can give them milk by spoon, cup, tube, at the breast, or bottle.
If you are supplementing your baby’s feeds, or entirely bottle feeding, it’s important to be guided by tummy sizes, normal breastfeeding volumes, normal length of breastfeeds (around 15-20 mins) and your baby’s feeding and satisfaction cues. Calculations using formulas such as mls/kg/day are guides for when fluid requirements (often IV fluids) are needed, and when you can’t rely on your baby’s normal signs of feeding and looking full.
Giving your baby infant formula is usually not the answer. It’ll decrease the time they spend at your breast and interfere with supply and demand, which leads to slower milk production. Rather than giving your baby infant formula, the World Health Organization (WHO) says it is better to give breastmilk from another healthy mother. What you feed your baby is always your choice.
The Australian Breastfeeding Association has more helpful info on this topic here.
How do I hand express my breastmilk?
How to hand express
1) Wash your hands.
2) Gently massage your breasts and areola (the coloured area on the breast around the nipple). Using warmth is helpful (like in the shower).
– Put your finger and thumb on opposite sides of your breast about 2-3 cm away from the nipple.
– Push back into your chest (Don’t stretch your fingers out)
– Roll finger and thumb together. Avoid pulling, squeezing or sliding.
– Then relax your fingers and repeat.
Repeat many times in a rhythmic way. It may take some time for milk to flow. In the early days there will only be drops.
3) After a few minutes rotate the position of your fingers.
4) Relaxing, visualising the milk flowing, thinking about your baby, doing more massage and changing breasts, all help the milk to flow.
Like most things, it gets easier with practice! If you wish to collect your milk, use a clean container, such as a small bowl or cup.
What are breast compressions?
Breast compressions are a squeeze and hold technique. You can take a handfull of your breast between your fingers and thumb, or use the flat of your hand. It’s not massage or stroking. Think of your breast as an icing bag and you are squeezing the icing out!
Breast compressions are helpful when:
- you are experiencing small volumes of colostrum or milk
- your baby is getting tired
- your milk flow is slowing down
- you want your baby to get the ‘last drops’ of creamy milk.
Concerns and challenges
My nipples are sore
Nipples are sensitive during pregnancy and in the early days of breastfeeding due to hormones. The sensitivity usually goes away by about two weeks after birth.
It can be normal to have some discomfort at the beginning of feeds as your baby latches and your nipple is stretched. What’s not normal is experiencing pain through the entire feed, or for your nipple to look out of shape afterwards.
If you experience lots of pain, and/or nipple damage, don’t suffer, get help from your midwife or a lactation consultant. There are many different causes of sore nipples, and many ways to help. Here are some ways you can reduce nipple pain and damage for a more comfortable and enjoyable feed for both you and your baby.
- Help your baby get a big mouthful of breast, not just the nipple.
- Shape your breast like you might squish a burger.
- Try a different position, especially getting your baby more on their tummy to help them get a bigger mouthful.
- Once your baby is latched, you can sometimes pull on the chin and get a wider open mouth.
- Check that your nipple is not getting bent during feeds. Look for a nipple pointing to the side, or a crease at the base of the nipple the moment the nipple is released. This often happens when the ‘cross cradle’ position is used and the baby’s head gets tilted, or a little ‘around to the side’, or with the nose and not the chin being closest to the breast.
- If you’re taking your baby off the breast, make sure you break the suction with your finger first.
- Breastmilk left to dry on the nipple is healing, so is olive oil and coconut oil.
- You can take paracetamol or ibuprofen (hardly any gets through to the baby).
- Avoid nipple creams as there’s little evidence they help. Lanolin and hydrogel pads have been found to be associated with infections, particularly thrush.
- Wash your nipples with mild soap and apply saline (½ tsp salt in a cup of water) which has been found to reduce infection.
- Wet green tea bags are also helpful.
- Nipples do best when they are not squashed and get some light and air.
Here are some more resources on how you can care for your nipples:
Sore nipples or breasts
Care of nipples while breastfeeding
Are there any cures for sore nipples
Topical treatment for nipples
Does lanolin increase the risk for infection
I have burning, stabbing, shooting nipple pain. Could it be thrush?
Thrush is an imbalance of the normal bacteria
Signs of thrush
- Your nipples are very tender to touch and even light clothing can cause pain.
- You may have stinging nipple pain during and after
- Your nipples may be bright pink and/or shiny and the areola may be reddened, dry or slightly flaky.
- Your breasts may have shooting, stabbing, or deep aching pain. It might radiate into your back or down your arm. It’s often during letdown and afterfeeding or expressing.
- The pain may be one side or both.
- Your breasts will look and feel normal (not with a hard and/or red area like with mastitis).
- You may have had antibiotics recently (which can increase your risk of thrush).
If you have been diagnosed with nipple thrush…
- your lead maternity carer (LMC) or doctor may prescribe medication.
- apply Miconazole oral gel/cream or Nystatin cream after each feed (or 3-4 hourly during the day). You don’t need to wipe the gel/cream from the nipples before the next feed.
- your baby will need to be treated too. You can apply oral gel to your baby’s mouth.
- expose your nipples to air and sunlight (as much as possible!)
- you can take ibuprofen or paracetamol for your pain
- get help if your nipple pain and damage does not improve after a few days
- sometimes a repeat prescription is needed, especially if the pain involves the whole
It’s best to avoid…
- lanolin and other nipple ointments (other than those mentioned earlier)
- nursing/breast pads
- tight, synthetic bras and clothing
- wearing a bra at night
- consuming large amounts of sugars, honey, artificial sweeteners, carbohydrates, dairy products (except yoghurt with live cultures) yeasts (including brewer’s yeast and vitamin B supplements), alcohol, fermented foods
- using anti-bacterial soap – just use a regular soap (you want to keep your normal bacteria)
- dummies/pacifiers.
Try to…
- improve your diet and treat any deficiencies of vitamins A, B, C, and K, folic acid, iron, and zinc
- wash your hands after handling your breasts or breastmilk, changing nappies and using the toilet
- use the hottest wash and hang out your laundry in the sun
- use the hottest wash for dishes
- sterilise by boiling any toys, teats, pacifiers, teethers, pump parts
- treat any nappy rash, vaginal thrush, tinea.
Using distilled vinegar (heat treated to remove mould spores) and water solution to add to baths, final rinses of washing machines and directly on affected or at-risk skin can also be effective. The resulting pH change makes yeast production less likely.
Yeast infections and the breastfeeding family
My breasts feel uncomfortably full. What can I do?
Uncomfortably full breasts can start a few days after the birth of your baby. It’s important to relieve the fullness however you can. The best way is to feed your baby often.
Here are some solutions to relieve breast engorgement or full breasts;
-
- wake your baby for a feed or hand express
- if your breasts are too full for your baby to latch on well, express some milk before trying again
- use your fingers on the areola area to push back and hold for a moment or two immediately before latching. This will help push some of the swelling away and make it easier to latch
- if your baby doesn’t feed and relieve some fullness, hand express until your breasts have softened and you are comfortable
- after feeds use something cold on your breasts.
- you can take ibuprofen or paracetamol.
- wearing a supportive bra may help, or you may prefer to not wear one at all.
- spend some time gently massaging away from the nipple and towards the armpit. There can be a lot of fluid (not milk) that needs to drain away. You might like to massage with some oil while lying on your back. In some cultures, this breast massage is a normal part of a woman’s care during this time.
- see Full Breasts.
- contact your lead maternity carer (LMC) for help and support.
I have painful breasts. Do I have a plugged duct or mastitis?
What’s mastitis?
If your breasts are painful and reddened and you feel unwell with flu-like symptoms, you’re likely experiencing a breast infection called mastitis. You may have a fever and feel dreadful. This sometimes happens around 2-3 months but can happen at other times too. It is connected with an over production of milk, sore and damaged nipples, and an imbalance in the normal bacteria in and around the breast.
Sometimes an area of your breast hasn’t drained well. Maybe your baby’s position wasn’t the best and your nipple was a little bent, reducing the flow from an area. This makes the breast inflammed and then the flow is reduced. This can be known as a blocked duct.
Sometimes a small plug can cause a blockage in the nipple. You can see this as a white dot called a bleb. You can usually squeeze it out. It’s important to get the milk moving asap.
If you’ve got mastitis, it is important to:
- be very gentle with your breast and avoid firm massage
- avoid heat, instead cool your breast
- continue to breastfeed normally
- take anti-inflammatory medication eg Ibuprofen
- Rest
- Eat well and drink plenty of water
See Breast Care and Mastitis for more information.
If after about 12 – 24 hours you’re not feeling better, consult your midwife or doctor. You may need antibiotics.
Why doesn’t my baby want to breastfeed?
My baby fights the breast
If your baby is not in the right position, some of their reflexes can look like pushing, punching, ‘head-butting’ and turning away. It’s like your baby doesn’t want to feed when actually it’s the opposite.
If your hands are holding your baby’s head or neck it can be uncomfortable for your baby, and difficult to drink well too, so they may fuss.
Lean back so your baby is more on their tummy and able to move their head.
My baby fusses, pulls off or cries
If the milk flow is too fast or too slow, babies will fuss and pull off and sometimes cry.
If you think they are fussy because the flow is a bit slow, squeeze and hold your breast while your baby feeds. This will help your baby get the milk faster. You can also change sides often as this makes more milk available.
If you think the flow is a bit fast for your baby, it is best to lean back and have your baby more on top of you. That way your baby will cope with it better and not feel like they are drowning in it!
If your baby has a tongue restriction, both a slow flow and a fast flow will be more difficult to manage.
There are other reasons a baby fusses at the breast. You can find lots of help here or watch this short video.
How do I increase my milk production?
- Remove milk more often… by breastfeeding, hand expression or pumping.
- Help your baby get a good mouthful of breast.
- Help your baby be in a good drinking position… in close, tummy to tummy, chin in breast, head back.
- Squeeze and compress your breasts to help your baby get the milk.
- Swap sides often.
- Eat well, including protein and complex carbohydrates like oats.
- Drink enough fluids.
- Rest, relax, sleep when baby sleeps.
- Make sure you are not doing the things that slow production like poor diet, not enough rest, too much caffeine or stress, smoking, and certain medications.
- There are also herbs and medicines that help.
- Spend as much time as you can with your baby skin to skin and avoid long periods of separation if possible.
More Milk Out = More Milk Made
Emptier breasts make milk faster
Frequent milk removal = fast milk production
Fuller breasts make milk slower
Infrequent milk removal = slow milk production
If you’re still worried, please talk to your midwife, or a lactation consultant. We’re here to help.
How do I know if my baby is getting enough hind milk?
Foremilk is the milk your pēpi (baby) gets at the start of a feed; hindmilk is what they get towards the end of their feed. Generally, hindmilk has a higher fat content than foremilk. Over the course of a feed, your pēpi will consume all the foremilk and hindmilk they need.
Breast massage and compressions can increase the fat that a baby gets from the beginning of a feed. But trying to get more fat by restricting a baby to one breast only per feed or going back to the same breast for a specified time, can slow the overall milk production and result in baby getting less fat too in the end.
There’s no need to worry about hind milk. The fat content evens out between feeds and it’s the overall volume of milk that counts. Up to six months, breastmilk is 7.4% fat, but after 12 months it is 10.7%!
I think I have too much milk
Full breasts, leaking breasts, a strong let-down which causes your baby to cough and splutter, explosive frothy green poo, baby spilling lots, and appearing uncomfortable with gas, can all be caused by things other than having too much milk.
Sometimes in the early weeks there can be a little oversupply, but it usually settles on its own. But if these things above are a problem, and your baby’s weight gains are massive, you may benefit from slowing the milk production.
See this table for the weight gain you can expect
If you do need to reduce your production, you can feed your baby from one breast only. Or you can sometimes feed your baby from the same breast for around three or four hours. Be careful not to overdo this, because you don’t want to reduce the milk production too much or risk mastitis.
Restricting feeds in this way for a week should be enough.
How does milk production slow down?
Removing milk less often
This happens by:
- postponing or making baby wait for feeds
- feeding from one side only every feed
- getting baby to suck on a dummy
- baby having a long stretch of sleep, such as five hours at night,
- trying to get into ‘a routine’ rather than responding to baby’s feeding cues, or sleep training.
Removing milk less efficiently
This happens when:
- you limit the feed time
- baby doesn’t have a big mouthful of breast
- baby is not in a comfortable position to swallow easily (their chin is not touching your breast or maybe their body is twisted)
- the position of your baby’s head is making your nipple slightly bent – reducing milk flow)
- there’s some tongue restriction due to tongue tie or some other problem
- mum is very anxious or stressed which can make it difficult to let-down because adrenalin inhibits the hormone oxytocin.
Other things that can slow milk production:
- dieting
- smoking and alcohol
- lots of vigorous exercise
- being unwell
- hormonal contraception before milk production is really well-established
- cold and flu medications designed to dry up secretions.
All these factors affect women and babies differently.
My baby prefers one side
This is common in newborns. Many newborns come out a little ‘wonky’ because they’ve been growing in a very tight space. Sometimes they come out a little tighter and stronger on one side of their face and neck than the other. You might notice your baby’s head keeps turning to one side. Sometimes their jaw is a little crooked too. This can make feeding off one side easier than the other.
- Support your baby to find a position they can feed well in.
- Helping your baby change what side their head rests on when sleeping, and in the car seat, is a good idea.
- Make sure your baby has plenty of safe tummy time while they are awake. You can read more about this here:
A baby will also fuss at a breast when the milk flow is slow. If milk production on one side has become less, so will the flow.
If you are worried, please talk to your midwife or lactation consultant.
Tummy Time
Growing with good alignment
My baby throws up
Spitting up or spilling is very common and often happens when babies are burped. Babies aren’t usually bothered by their spitting up.
Babies spit up when they’ve taken more milk than their tummy can hold.
Smaller frequent feeds may result in less milk coming back up and will also mean the tummy contents are less acid.
Vomiting is forceful. If your baby is vomiting talk to your health professional.
When will my baby sleep?
Not sleeping in the bassinet is normal behaviour for a newborn. Your baby has only ever known the feeling and comfort of being surrounded by your body. Every single moment they got to enjoy your warm body contact, your smell, the sounds of your body, and its movement.
But now everything is different. Your baby will want to be close to you all the time. After a few days, your baby will have adjusted a bit and will often be ‘milk drunk’ after a feed. This makes settling in the bassinet a little more Safe co-sleeping devices including wahakura and pēpi pods are also suitable sleeping options. You can read the Ministry of Health’s safe sleeping guidelines here.
What’s normal?
- babies waking at night
- babies feeding often to get what they need for their tiny tummies
- sucking to sleep
- babies waking for many reasons, and needing help to get back to sleep
- a night feed is usually needed to maintain milk production.
Below is a selection of useful reading and viewing around sleeping:
Should babies sleep through the night?
Sleeping through the night
The baby sleep info source
Babies usually get the sleep they need – it just might not be as much as parents would prefer! But in time, your baby will stop waking at night even if you do nothing. Mothers who exclusively breastfeed usually have more and better-quality sleep, compared to those using formula or mixed feeding.
My baby cries a lot
Giving your baby your breast can be an excellent way to comfort them, whether they are hungry, thirsty or need your reassurance, contact, warmth, or something else. Sometimes babies will still cry after a feed – there are many reasons to explore why this may be happening.
But some babies cry a lot. See below to learn more about crying, and soothing techniques.
Your baby’s crying can be difficult to deal with, especially when you are stressed and tired. See here for important information on ways to help your baby, and yourself.
Coping with disrupted sleep or sleep deprivation
Sleep deprivation can be one of the biggest challenges that parents face. Be kind to yourself, ask for support so you can share the care of your baby, try and nap during the day when baby sleeps and get some fresh air if you can. Here are some other ways you can support yourself when you are feeling tired and sleep deprived;
Sleep deprivation and parenting
Caring for your baby at night
Many mothers and babies co-sleep at some time in their parenting journey. If you choose to co-sleep, there are ways to make it safer.
Co-sleeping
The Safe Sleep Seven
Safe Infant sleep book and other resources
Does sleep training work?
Sleep training is getting your baby to fall asleep on their own using different techniques, such as letting your baby cry without being comforted, either for gradually increasing periods of time or until they fall asleep.
Sleep training can be done through a sleep consultant. However, the sleep consultant industry is unregulated.
Sleep training can be stressful for both you and your baby.
- Results may not last and training is likely to need to be repeated, such as after teething or illness.
- It may have negative consequences for breastfeeding.
- It may have longer term or ‘bigger picture’ type consequences.
Babies and Sleep. A Matter of Choice
Baby sleep trainers do you have the guts to tell them to bugger off?
Families often turn to sleep training if they have unrealistic expectations about babies sleep, they feel pressured by others, or tiredness has them feeling desperate. Trying to manage non-stop crying, sleep deprivation and stressors both at home and outside is a lot to handle and increases the risk of violent behaviour. Shaking a baby is never okay and can result in debilitating or fatal injuries.
If you’re worried about your thoughts or feel you may be at risk of harming yourself or your baby, arrange an urgent appointment with your midwife or GP who can refer you for further support. You can also call Plunketline or Healthline 24 hours a day for support and advice
Healthline 0800 611 116 (24 hours a day; every day)
PlunketLine 0800 933 922 (24 hours a day; every day)
Often the shaker is not the biological parent but someone else caring for the baby – a boyfriend, step-parent, relative or someone else. That’s why it’s so important that parents are aware of the stress caregivers may feel when faced with a baby who seems to be crying nonstop. Everyone who cares for a baby needs to know the signs of increasing stress and where to get help.
Here is a useful link on how to stay calm with kids: Staying Calm With Kids
Below is important information on a baby’s development and mental health.
The Importance of Relationship Building
Controlled crying
Responding to baby’s cues
Building a Happy Baby
My baby sucks for a few minutes and then falls asleep … but as soon as I take him off he/she shows cues again!
Babies will do this when the flow is slow and are taking a break to conserve their energy. Sometimes a baby will look like they are asleep but if you notice their fists, you will see them tightly clenched. This is a tense baby taking some ‘time out’ to rest, not a baby who is done feeding.
- Squeezing and compressing your breast will get a little milk to flow and this usually gets a baby feeding again. This is so much more effective (and kinder) than blowing on, tickling or using other ways of harassing a baby to feed.
- Continuing to compress your breasts while your baby sucks, will help your baby get milk.
- Swap sides when there is an opportunity.
- Watch for those little fingers to unfurl and then the whole arm to become floppy and relaxed.
If you have lots of milk and a strong let-down causing the milk to flow rapidly, it’s possible for a baby to have a feed very quickly (and then fall asleep). But in this situation, you would notice very active feeding with lots of rapid, obvious swallows – not just sucking, then baby would take him/herself off the breast looking full and satisfied… with a floppy and relaxed arm.
My baby is using me ‘like a dummy’
For a baby, the breast is not just about food, but so much more. It’s a place of warmth, comfort, and connection. It’s where a baby loves to be, so they want to spend a lot of time there. Providing a little comfort in this way becomes one of the most rewarding (not to mention instant and highly effective) aspects of the breastfeeding experience.
- Maybe you are noticing that your baby is sucking but not swallowing. This may be because most of the milk has been removed from that breast. Maybe it is time to use Breast Compressions or swap sides.
- When you are noticing your baby sucking and it’s ‘fluttery’ in nature, this is what happens when a baby is drifting off to sleep.
Or maybe your baby is wanting to be at the breast when you feel your baby has had a good feed and can’t be hungry. Maybe your baby is still hungry. - You can’t spoil your baby by offering the breast whenever you notice their hunger cues. By letting your baby suck frequently at the breast, especially during the first weeks, you are establishing good milk production. Not letting your baby have the breast can delay this.
- Dummies are an attempt to provide a breast substitute, not the other way around. The baby should only ever use the breast like a breast.
My baby is ‘snack feeding’
– Babies often cluster feeds together and it can seem like a breastfeeding marathon.
– Newborns feed the most between 9pm and 3am; older babies usually feed earlier in the evening or late afternoon. This is normal and helps increase your milk production.
– Newborns then feed the least between 3am and 9am. They often have some good stretches of sleep then and it may be your best opportunity to catch up on your own sleep.
- Using Breast Compressions and swapping sides when you notice there aren’t many swallows, will help your baby make the most of their time at your breast.
- 8-12 feeds (or more), taking about 30 minutes (each 24 hours) is a normal beginning breastfeeding pattern.
- By responding to cues and feeding often, your milk production will meet your baby’s needs sooner and then the feeds may become less frequent. The feeds are also likely to become quicker.
‘Endless feeding’ can be a symptom of a tongue tie. Or there could be other issues. If you are concerned, talk to your midwife or lactation consultant.
Stretching out feed times and forcing routines
Your baby’s feeds, awake times, and sleep times will, over time, develop into something of a pattern. But no two days will be the same. Your baby will be growing, developing and changing every day.
Trying to manipulate feeding and sleeping times may not work and is not a good idea. It may result in less breastmilk production. Responding to your baby’s cues is much better for developing your bond and stimulating your milk production.
Stretching out feed times UNICEF
I think my baby is reacting to something in my milk
Windiness, tummy aches and unsettled behaviour are all a normal part of life with a young baby. Swallowing air when the milk flow is fast and a poor latch can worsen these symptoms or behaviours.
Your baby’s tummy and gut are immature – the best remedy is time. It’s usually nothing to do with the milk itself.
But sometimes babies can be allergic and react to something in the milk. These babies seem to vomit a lot, have lots of mucousy green explosive poos, have really rashy, spotty skin, are unhappy and not growing so well. Sometimes eliminating certain foods from your diet can help.
Again, sometimes eliminating certain foods from your diet can help.
What about allergies?
The latest guidelines from The Centre for Food and Allergy Research (CFAR) and The Australasian Society of Clinical Immunology and Allergy (ASCIA) are…
- When your baby is ready, at around six months, but not before four months, start to introduce a variety of solid foods, starting with iron rich foods, while continuing breastfeeding.
- All babies should be given allergenic solid foods including peanut butter, cooked egg, dairy and wheat products in the first year of life. This includes infants at high risk of allergy.
- Hydrolysed (partially or extensively) infant formula are not recommended for prevention of allergic disease.
Although your baby is likely to be taking increasing amounts of solids, breastmilk remains an important food for your baby.
New Recommendations for infant feeding
UNICEF – Allergies
Eat peanuts during pregnancy and breastfeeding to reduce peanut sensitisation in your child
A Joint Statement from the Scientific Advisory Committee on Nutrition and the Committee on Toxicity of Chemicals in food, Consumer products and the Environment
Media Release – Great result for Infant Feeding Guidelines consensus
Should I give my baby ‘Follow On’ formula?
The World Health Organization says follow-on formula is not necessary and is unsuitable as a breast-milk replacement from six months of age onwards. It says current formulations lead to a higher protein intake and lower intake of essential fatty acids, iron, zinc and B vitamins than recommended for adequate growth and development. It is especially unsuitable for babies less than six months of age.
When your baby is a year old they can have regular cow’s milk or plant-based milk, as well as breastmilk and family foods, but there is no need for infant formula of any kind.
WHO states that follow-up formula is not necessary and that marketing may mislead parents
Information concerning the use and marketing of follow-up formula
Infant Formula marketing practices that endanger our children
WHO/UNICEF information note: cross-promotion of infant formula and toddler milks
Going Back to Work
What are my rights around breastfeeding and work?
Many women breastfeed and work
The Human Rights Act says it is illegal for someone to stop you breastfeeding at work, where you are studying, on public transport, in government departments, in public places and in restaurants and shops… anywhere you are entitled to be.
From 1st July 2020, paid parental leave increased from 22 to 26 weeks. You can find out more and calculate your entitlements here.
By law, your employer must give you unpaid breaks to breastfeed your baby or express milk at work and provide you with a clean and private space to do this. You will need somewhere to sit, and you might ask for access to a power point to pump and a fridge to store the milk.
Breastfeeding breaks are to be provided in addition to the standard paid rest breaks and unpaid meal breaks. The rest and meal breaks can also be used as breastfeeding breaks if both the employer and employees agree to this.
You can find the latest information here.
Here is some further information on your rights and returning to work:
- Your rights as a breastfeeding mother
- Your rights as a breastfeeding mother – te reo Māori
- Breastfeeding and returning to work
- Breastfeeding Friendly Workplaces
- Guidance on supporting breastfeeding mothers returning to work
- What are womes ‘rights’ when it comes to infant feeding – an article by Professor Amy Brown
How do I keep breastfeeding while working?
Using a pump once or twice while at work is one way to keep your milk production going well and provide milk for your baby. You might want to practise pumping before you return to work.
How much milk will my baby need?
It depends how long you’re away from your baby. And how often your baby might want to feed (which can be a little more difficult to predict).
- From about 1-2 weeks onwards, the ‘average’ amount breastfed babies have in total each 24 hours is 750 ml, (ranging between 570-900 ml).
- The average number of feeds is ten.
- The average amount each feed is about 75mls.
- By the time a baby is about six months old the ‘average’ amount of breastmilk taken has increased to become about 900 mls each 24 hours.
- A feed (full tummy) for a week-old baby could be about 45-60 ml.
- A feed (full tummy) for a month-old baby could be about 80-150 ml.
Many babies will take only small amounts of breastmilk from a bottle or cup, but once back with mum, will feed lots. It’s not likely to matter.
Here’s some helpful info on how much expressed milk your baby might need: How much expressed milk will my baby need?
How do I use a Breast Pump? How do I pump more milk?
There are many times when using hand expression or pumping can be helpful. These may include:
- if your baby is having difficulty latching on, or getting milk from the breast
- to stimulate milk production
- relieving fullness or engorgement
- if you have a premature baby
- if you and your baby are separated for some reason
- if you are returning to work or need to go out without your baby.
You can get milk by hand or use a pump… whatever works best for you.
Using a breast pump
There are all sorts of pumps available. Whatever type you use, you will get more milk if you use your hands to compress and squeeze your breasts. Some mums find they don’t get much when using a pump. Don’t worry, it’s not always a good indication of the amount available. It’s helpful to respond to your pump as if it’s your baby, so the oxytocin flows.
Your lead maternity carer (LMC) or local breastfeeding support can give you advice on how to access a breast pump suitable for your needs.
See here for How to pump lots of breastmilk
How long can I store my breastmilk?
Breastmilk can be stored for days in the fridge and months in the freezer.
It’s better to store it at the back and bottom of your fridge, rather than in the door. Store breastmilk in small quantities to avoid waste.
Thaw and heat the amount of milk needed for a feed by standing the container in warm water.
Don’t use the microwave for thawing or heating breastmilk as this can alter special properties in the milk and may heat the milk unevenly.
Frozen breastmilk should be used within 24 hours of defrosting.
How do I give my baby a bottle?
If you provide bottles for caregivers to feed your baby with while you are away, it’s helpful if they know how to give a feed that, as much as possible, is like breastfeeding. Explaining to your baby’s caregivers about ‘Paced Bottle Feeding’ will help.
Paced feeding will also help ensure that the volumes given are manageable for you to keep up with. It will also lessen your baby’s frustration when back feeding at the breast.
How to pace bottle feed a baby
You don’t have to use a bottle. Milk can also be given by cup (even newborns). Cup feeding a newborn